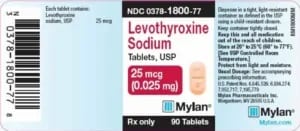
Levothyroxine sodium (generic) tablets for oral use
Summary about Levothyroxine sodium (generic) tablets for oral use
Levothyroxine sodium tablets, for oral use is a prescription, man-made thyroid hormone that is used to treat a condition called hypothyroidism. Levothyroxine sodium tablets contain synthetic crystalline L-3,3′,5,5′-tetraiodothyronine sodium salt [levothyroxine (T4) sodium] as an active ingredient. Synthetic T4 is chemically identical to the hormone produced in the human thyroid gland.

Levothyroxine sodium is a generic product meaning that it is a pharmaceutical drug that contains the same chemical substance as a drug that was originally protected by chemical patents. Generic drugs are allowed for sale after the patents on the original drugs expire. Because the active chemical substance is the same, the medical profile of generics is equivalent in performance. A generic drug has the same active pharmaceutical ingredient (API) as the original, but it may differ in some characteristics such as the manufacturing process, formulation, excipients, color, taste, and packaging.
Levothyroxine sodium tablets for oral administration are supplied in the following strengths: 25 mcg, 50 mcg, 75 mcg, 88 mcg, 100 mcg, 112 mcg, 125 mcg, 137 mcg, 150 mcg, 175 mcg, 200 mcg, and 300 mcg.
Generally, thyroid replacement treatment is to be taken for life. Levothyroxine sodium should not be used to treat noncancerous growths or enlargement of the thyroid in patients with normal iodine levels, or in cases of temporary hypothyroidism caused by inflammation of the thyroid gland (thyroiditis).
Important safety informations
Thyroid hormones, including Levothyroxine sodium, should not be used either alone or in combination with other drugs for the treatment of obesity or weight loss. In patients with normal thyroid levels, doses of Levothyroxine sodium used daily for hormone replacement are not helpful for weight loss. Larger doses may result in serious or even life-threatening events, especially when used in combination with certain other drugs used to reduce appetite.
Do not use Levothyroxine sodium if you have uncorrected adrenal problems.
Taking too much levothyroxine has been associated with increased bone loss, especially in women after menopause.
Once your doctor has found your specific Levothyroxine sodium dose, it is important to have lab tests done, as ordered by your doctor, at least once a year.
Foods like soybean flour, cottonseed meal, walnuts, and dietary fiber may cause your body to absorb less Levothyroxine sodium from the gastrointestinal tract. Grapefruit juice may cause your body to absorb less levothyroxine and may reduce its effect. Let your doctor know if you eat these foods, as your dose of Levothyroxine sodium may need to be adjusted.
Use Levothyroxine sodium only as ordered by your doctor. Take Levothyroxine sodium as a single dose, preferably on an empty stomach, one-half to one hour before breakfast.
Products such as iron and calcium supplements and antacids can lower your body’s ability to absorb levothyroxine, so Levothyroxine sodium should be taken 4 hours before or after taking these products.
Tell your doctor if you are pregnant or breastfeeding or are thinking of becoming pregnant while taking Levothyroxine sodium. Your dose of Levothyroxine sodium may need to be increased during your pregnancy.
It may take several weeks before you notice an improvement in your symptoms.
Tell your doctor about any other medical conditions you may have, especially heart disease, diabetes, blood clotting problems, and adrenal or pituitary gland problems. The dose of other drugs you may be taking to control these conditions may have to be changed while you are taking Levothyroxine sodium. If you have diabetes, check your blood sugar levels and/or the glucose in your urine, as ordered by your doctor, and immediately tell your doctor if there are any changes. If you are taking blood thinners, your blood clotting status should be checked often.
Tell your doctor or dentist that you are taking Levothyroxine sodium before any surgery.
Tell your doctor if you develop any of the following symptoms: rapid or abnormal heartbeat, chest pain, difficulty catching your breath, leg cramps, headache, nervousness, irritability, sleeplessness, shaking, change in appetite, weight gain or loss, vomiting, diarrhea, increased sweating, difficulty tolerating heat, fever, changes in menstrual periods, swollen red bumps on the skin (hives) or skin rash, or any other unusual medical event.
Partial hair loss may occur during the first few months you are taking Levothyroxine sodium.
Levothyroxine sodium (levothyroxine sodium) |
|
Active Ingredient |
Levothyroxine sodium |
Administration Route |
Tablets for oral use |
Alcohol Warning |
There is no interaction between alcohol and levothyroxine sodium |
Available Strength |
Tablets: 25, 50, 75, 88, 100, 112, 125, 137, 150, 175, 200, and 300 mcg |
Breastfeeding Warning |
Although levothyroxine sodium is excreted into human milk, use is considered acceptable.
-Levothyroxine (T4) is a normal component of human milk; limited data on exogenous replacement doses during breastfeeding have not shown an adverse effect in nursing infants. |
Clinical Pharmacology |
Pharmacodynamics
Oral levothyroxine sodium is a synthetic T4 hormone that exerts the same physiologic effect as endogenous T4, thereby maintaining normal T4 levels when a deficiency is present. Pharmacokinetics Absorption Absorption of orally administered T4 from the gastrointestinal tract ranges from 40% to 80%. The majority of the LEVOTHYROXINE SODIUM dose is absorbed from the jejunum and upper ileum. The relative bioavailability of LEVOTHYROXINE SODIUM tablets, compared to an equal nominal dose of oral levothyroxine sodium solution, is approximately 93%. T4 absorption is increased by fasting, and decreased in malabsorption syndromes and by certain foods such as soybeans. Dietary fiber decreases bioavailability of T4. Absorption may also decrease with age. In addition, many drugs and foods affect T4 absorption. Distribution Circulating thyroid hormones are greater than 99% bound to plasma proteins, including thyroxine-binding globulin (TBG), thyroxine-binding prealbumin (TBPA), and albumin (TBA), whose capacities and affinities vary for each hormone. The higher affinity of both TBG and TBPA for T4 partially explains the higher serum levels, slower metabolic clearance, and longer half-life of T4 compared to T3. Protein-bound thyroid hormones exist in reverse equilibrium with small amounts of free hormone. Only unbound hormone is metabolically active. Many drugs and physiologic conditions affect the binding of thyroid hormones to serum proteins. Thyroid hormones do not readily cross the placental barrier. Elimination Metabolism T4 is slowly eliminated. The major pathway of thyroid hormone metabolism is through sequential deiodination. Approximately 80% of circulating T3 is derived from peripheral T4 by monodeiodination. The liver is the major site of degradation for both T4 and T3, with T4 deiodination also occurring at a number of additional sites, including the kidney and other tissues. Approximately 80% of the daily dose of T4 is deiodinated to yield equal amounts of T3 and reverse T3 (rT3). T3 and rT3 are further deiodinated to diiodothyronine. Thyroid hormones are also metabolized via conjugation with glucuronides and sulfates and excreted directly into the bile and gut where they undergo enterohepatic recirculation. Excretion Thyroid hormones are primarily eliminated by the kidneys. A portion of the conjugated hormone reaches the colon unchanged and is eliminated in the feces. Approximately 20% of T4 is eliminated in the stool. Urinary excretion of T4 decreases with age. |
Cost |
Generic levothyroxine is covered by most Medicare and insurance plans, but some pharmacy coupons or cash prices may be lower. The lowest GoodRx price for the most common version of levothyroxine is around $10.00, 73% off the average retailprice of $38.07. |
Dosage Form |
Oral tablet |
Dose Schedule |
Administer once daily, preferably on an empty stomach, one-half to one hour before breakfast.
Administer at least 4 hours before or after drugs that are known to interfere with absorption. Evaluate the need for dose adjustments when regularly administering within one hour of certain foods that may affect absorption. Starting dose depends on a variety of factors, including age, body weight, cardiovascular status, and concomitant medications. Peak therapeutic effect may not be attained for 4-6 weeks. Adequacy of therapy determined with periodic monitoring of TSH and/or T4 as well as clinical status. |
Drug Class |
H03AA — Thyroid hormones |
Drug Unit |
mcg |
Food Warning |
Consumption of certain foods may affect LEVOTHYROXINE SODIUM absorption thereby necessitating adjustments in dosing. Soybean flour, cottonseed meal, walnuts, and dietary fiber may bind and decrease the absorption of LEVOTHYROXINE SODIUM from the gastrointestinal tract. Grapefruit juice may delay the absorption of levothyroxine and reduce its bioavailability. |
Included In
|
Generic levothyroxine is covered by most Medicare and insurance plans |
Interacting Drugs |
Drugs That May Decrease T4 Absorption (Hypothyroidism)
Calcium Carbonate and Ferrous Sulfate: Calcium carbonate may form an insoluble chelate with levothyroxine, and ferrous sulfate likely forms a ferricthyroxine complex. Administer LEVOTHYROXINE SODIUM at least 4 hours apart from these agents. Orlistat: Monitor patients treated concomitantly with orlistat and LEVOTHYROXINE SODIUM for changes in thyroid function. Bile Acid Sequestrants (Colesevelam, Cholestyramine, Colestipol) and Ion Exchange Resins (Kayexalate, Sevelamer): Bile acid sequestrants and ion exchange resins are known to decrease levothyroxine absorption. Administer LEVOTHYROXINE SODIUM at least 4 hours prior to these drugs or monitor TSH levels. Proton Pump Inhibitors, Sucralfate, Antacids, Aluminum & Magnesium Hydroxides and Simethicone: Gastric acidity is an essential requirement for adequate absorption of levothyroxine. Sucralfate, antacids and proton pump inhibitors may cause hypochlorhydria, affect intragastric pH, and reduce levothyroxine absorption. Monitor patients appropriately. Drugs That May Alter T4 and Triiodothyronine (T3) Serum Transport Without Affecting Free Thyroxine (FT4) Concentration (Euthyroidism) Clofibrate, Estrogen-containing oral contraceptives, Estrogens (oral), Heroin / Methadone, 5-Fluorouracil, Mitotane, Tamoxifen: These drugs may increase serum thyroxine-binding globulin (TBG) concentration. Androgens/Anabolics, Steroids, Asparaginase, Glucocorticoids, Slow-Release, Nicotinic Acid: These drugs may decrease serum TBG concentration. Potential impact: Administration of these agents with LEVOTHYROXINE SODIUM results in an initial transient increase in FT4. Continued administration results in a decrease in serum T4 and normal FT4 and TSH concentrations. Salicylates (> 2 g/day): Salicylates inhibit binding of T4 and T3 to TBG and transthyretin. An initial increase in serum FT4 is followed by return of FT4 to normal levels with sustained therapeutic serum salicylate concentrations, although total T4 levels may decrease by as much as 30%. Carbamazepine. Furosemide (> 80 mg IV), Heparin, Hydantoins, Non-Steroidal Anti-inflammatory Drugs, Fenamates: These drugs may cause protein-binding site displacement. Furosemide has been shown to inhibit the protein binding of T4 to TBG and albumin, causing an increase free T4 fraction in serum. Furosemide competes for T4-binding sites on TBG, prealbumin, and albumin, so that a single high dose can acutely lower the total T4 level. Phenytoin and carbamazepine reduce serum protein binding of levothyroxine, and total and free T4 may be reduced by 20% to 40%, but most patients have normal serum TSH levels and are clinically euthyroid. Closely monitor thyroid hormone parameters. Drugs That May Alter Hepatic Metabolism of T4 (Hypothyroidism) Phenobarbital, Rifampin: Phenobarbital has been shown to reduce the response to thyroxine. Phenobarbital increases L-thyroxine metabolism by inducing uridine 5’-diphospho-glucuronosyltransferase (UGT) and leads to a lower T4 serum levels. Changes in thyroid status may occur if barbiturates are added or withdrawn from patients being treated for hypothyroidism. Rifampin has been shown to accelerate the metabolism of levothyroxine. Drugs That May Decrease Conversion of T4 to T3 Beta-adrenergic antagonists (e.g., Propranolol > 160 mg/day): In patients treated with large doses of propranolol (> 160 mg/day), T3 and T4 levels change, TSH levels remain normal, and patients are clinically euthyroid. Actions of particular beta-adrenergic antagonists may be impaired when a hypothyroid patient is converted to the euthyroid state. Glucocorticoids (e.g., Dexamethasone > 4 mg/day): Short-term administration of large doses of glucocorticoids may decrease serum T3 concentrations by 30% with minimal change in serum T4 levels. However, long-term glucocorticoid therapy may result in slightly decreased T3 and T4 levels due to decreased TBG production. Other drugs: Amiodarone Amiodarone inhibits peripheral conversion of levothyroxine (T4) to triiodothyronine (T3) and may cause isolated biochemical changes (increase in serum free-T4, and decreased or normal free-T3) in clinically euthyroid patients. Antidiabetic Therapy Addition of LEVOTHYROXINE SODIUM therapy in patients with diabetes mellitus may worsen glycemic control and result in increased antidiabetic agent or insulin requirements. Carefully monitor glycemic control, especially when thyroid therapy is started, changed, or discontinued. Oral Anticoagulants LEVOTHYROXINE SODIUM increases the response to oral anticoagulant therapy. Therefore, a decrease in the dose of anticoagulant may be warranted with correction of the hypothyroid state or when the LEVOTHYROXINE SODIUM dose is increased. Closely monitor coagulation tests to permit appropriate and timely dosage adjustments. Digitalis Glycosides LEVOTHYROXINE SODIUM may reduce the therapeutic effects of digitalis glycosides. Serum digitalis glycoside levels may decrease when a hypothyroid patient becomes euthyroid, necessitating an increase in the dose of digitalis glycosides. Antidepressant Therapy Concurrent use of tricyclic (e.g., amitriptyline) or tetracyclic (e.g., maprotiline) antidepressants and LEVOTHYROXINE SODIUM may increase the therapeutic and toxic effects of both drugs, possibly due to increased receptor sensitivity to catecholamines. Toxic effects may include increased risk of cardiac arrhythmias and central nervous system stimulation. LEVOTHYROXINE SODIUM may accelerate the onset of action of tricyclics. Administration of sertraline in patients stabilized on LEVOTHYROXINE SODIUM may result in increased LEVOTHYROXINE SODIUM requirements. Ketamine Concurrent use of ketamine and LEVOTHYROXINE SODIUM may produce marked hypertension and tachycardia. Closely monitor blood pressure and heart rate in these patients. Sympathomimetics Concurrent use of sympathomimetics and LEVOTHYROXINE SODIUM may increase the effects of sympathomimetics or thyroid hormone. Thyroid hormones may increase the risk of coronary insufficiency when sympathomimetic agents are administered to patients with coronary artery disease. Tyrosine-Kinase Inhibitors Concurrent use of tyrosine-kinase inhibitors such as imatinib may cause hypothyroidism. Closely monitor TSH levels in such patients. |
Is Available Generically |
Yes. |
Is Proprietary |
No |
Label Details |
https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=5723c7a7-2a1d-4ab6-bf39-b2165ae781a6&type=display |
Legal Status |
Legal.
Is not subject to the Controlled Substances Act. |
Manufacturer |
Mylan Institutional Inc. |
Maximum Intake |
200 to 300 mcg/day |
Mechanism of Action |
Levothyroxine is a synthetically prepared levo-isomer of the thyroid hormone thyroxine (T4, a tetra-iodinated tyrosine derivative) that acts as a replacement in deficiency syndromes such as hypothyroidism. T4 is the major hormone secreted from the thyroid gland and is chemically identical to the naturally secreted T4: it increases metabolic rate, decreases thyroid-stimulating hormone (TSH) production from the anterior lobe of the pituitary gland, and, in peripheral tissues, is converted to T3. Thyroxine is released from its precursor protein thyroglobulin through proteolysis and secreted into the blood where is it then peripherally deiodinated to form triiodothyronine (T3) which exerts a broad spectrum of stimulatory effects on cell metabolism. T4and T3 have a relative potency of ~1:4.
Thyroid hormone increases the metabolic rate of cells of all tissues in the body. In the fetus and newborn, thyroid hormone is important for the growth and development of all tissues including bones and the brain. In adults, thyroid hormone helps to maintain brain function, food metabolism, and body temperature, among other effects. The symptoms of thyroid deficiency relieved by levothyroxine include slow speech, lack of energy, weight gain, hair loss, dry thick skin and unusual sensitivity to cold. The thyroid hormones have been shown to exert both genomic and non-genomic effects. They exert their genomic effects by diffusing into the cell nucleus and binding to thyroid hormone receptors in DNA regions called thyroid hormone response elements (TREs) near genes. This complex of T4, T3, DNA, and other coregulatory proteins causes a conformational change and a resulting shift in transcriptional regulation of nearby genes, synthesis of messenger RNA, and cytoplasmic protein production. For example, in cardiac tissues T3 has been shown to regulate the genes for α- and β-myosin heavy chains, production of the sarcoplasmic reticulum proteins calcium-activated ATPase (Ca2+-ATPase) and phospholamban, β-adrenergic receptors, guanine-nucleotide regulatory proteins, and adenylyl cyclase types V and VI as well as several plasma-membrane ion transporters, such as Na+/K+–ATPase, Na+/Ca2+ exchanger, and voltage-gated potassium channels, including Kv1.5, Kv4.2, and Kv4.3. As a result, many cardiac functions including heart rate, cardiac output, and systemic vascular resistance are closely linked to thyroid status. The non-genomic actions of the thyroid hormones have been shown to occur through binding to a plasma membrane receptor integrin aVb3 at the Arg-Gly-Asp recognition site. From the cell-surface, T4 binding to integrin results in down-stream effects including activation of mitogen-activated protein kinase (MAPK; ERK1/2) and causes subsequent effects on cellular/nuclear events including angiogenesis and tumor cell proliferation.
|
Non Proprietary Name |
Levothyroxine sodium |
Overdosage |
The signs and symptoms of overdosage are those of hyperthyroidism. In addition, confusion and disorientation may occur. Cerebral embolism, shock, coma, and death have been reported. Seizures occurred in a 3-year-old child ingesting 3.6 mg of levothyroxine. Symptoms may not necessarily be evident or may not appear until several days after ingestion of levothyroxine sodium.
Reduce the LEVOTHYROXINE SODIUM dose or discontinue temporarily if signs or symptoms of overdosage occur. Initiate appropriate supportive treatment as dictated by the patient’s medical status. |
Pregnancy Category |
AU TGA pregnancy category A: Drugs which have been taken by a large number of pregnant women and women of childbearing age without any proven increase in the frequency of malformations or other direct or indirect harmful effects on the fetus having been observed.US FDA pregnancy category Not Assigned: The US FDA has amended the pregnancy labeling rule for prescription drug products to require labeling that includes a summary of risk, a discussion of the data supporting that summary, and relevant information to help health care providers make prescribing decisions and counsel women about the use of drugs during pregnancy. Pregnancy categories A, B, C, D, and X are being phased out. |
Pregnancy Warning |
Use is considered acceptable.
Risk Summary: No increased rates of major birth defects or miscarriages have been reported with use during pregnancy; untreated hypothyroidism during pregnancy is associated with risks to the mother and fetus. Thyroid replacement therapy should not be discontinued during pregnancy; hypothyroidism diagnosed during pregnancy should be promptly treated. Animal studies have not been conducted. There is a long history of using this drug in pregnant women and this experience has not shown increased rates of fetal malformations, miscarriages or other adverse maternal or fetal outcomes. Hypothyroidism during pregnancy is associated with a higher rate of complications, including spontaneous abortion, pre-eclampsia, stillbirth and premature delivery. Maternal hypothyroidism may have an adverse effect on fetal neurocognitive development. Pregnant women taking this drug should have their TSH measured during each trimester and dose adjusted as appropriate. Patients will generally return to their pre-pregnancy dose after delivery. There are no controlled data in human pregnancy. |
Prescribing Info |
https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=5723c7a7-2a1d-4ab6-bf39-b2165ae781a6&type=display |
Prescription Status |
Prescription drug |
Proprietary Name |
Levothyroxine sodium |
Related Drugs |
Tiratricol, Liothyronine |
RxCUI |
40144 |
Warning |
Cardiac adverse reactions in the elderly and in patients with underlying cardiovascular disease: Initiate LEVOTHYROXINE SODIUM at less than the full replacement dose because of the increased risk of cardiac adverse reactions, including atrial fibrillation.Myxedema coma: Do not use oral thyroid hormone drug products to treat myxedema coma.Acute adrenal crisis in patients with concomitant adrenal insufficiency: Treat with replacement glucocorticoids prior to initiation of LEVOTHYROXINE SODIUM treatment.Prevention of hyperthyroidism or incomplete treatment of hypothyroidism: Proper dose titration and careful monitoring is critical to prevent the persistence of hypothyroidism or the development of hyperthyroidism.Worsening of diabetic control: Therapy in patients with diabetes mellitus may worsen glycemic control and result in increased antidiabetic agent or insulin requirements. Carefully monitor glycemic control after starting, changing, or discontinuing thyroid hormone therapy.Decreased bone mineral density associated with thyroid hormone overreplacement: Over-replacement can increase bone resorption and decrease bone mineral density. Give the lowest effective dose. |
Links:
https://www.mylan.com/en/products/product-catalog/product-profile-page?id=a547811c-2e10-4d36-a809-7ddd2726e51a
https://www.drugs.com/levothyroxine.html
https://www.drugbank.ca/drugs/DB00451
https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=5723c7a7-2a1d-4ab6-bf39-b2165ae781a6